The UNSW Medicine program has a curriculum where medical science and clinical disciplines are highly integrated to ensure an optimum learning experience.
UNSW Medicine has developed an innovative six year, three Phase undergraduate Medicine program. The program leads to the awards of Bachelor of Medical Studies/Doctor of Medicine (BMed/MD).
The program has been developed to reflect dramatic changes in the environment of medical practice to meet:
Assessment of learning in the Medicine program has been designed to support and direct student learning. Key features of the system include:
An assessment system that is outcome or capability based, requiring students to demonstrate their ongoing development in the eight capability areas. Progression will not be based solely on satisfactory completion of individual courses, nor will it correspond solely to annual stages;
A focus on assessment for learning, with learning tasks, carried out individually or in groups, forming a significant part of the assessment, opportunities for formative assessment;
Coarse grading of summative assessments, with repeated sampling. Most assessments are graded on a four point scale;
Examinations that require students to integrate basic, clinical and social sciences; with no discipline-specific assessments;
Assessment of clinical skills during clinical placements as well as in formal clinical examinations (performance assessments);
A learning portfolio examination in each phase that requires students to collect evidence of their performances in specified areas of capability, select their best examples and submit these, together with a commentary on their learning, for review. In phase three this examination involves an oral defence;
Grading systems which are criterion referenced, making the expected standards of performance clear and explicit to students and to examiners alike;
Development of student autonomy in regard to assessment through involvement in some self and peer assessment, some negotiation of assignments and projects, and the process of selecting and reflecting on student's evidence for learning in the capabilities for the portfolio examinations.
These characteristics of the assessment scheme have been designed to encourage active learning and to support interdisciplinary integration.
A wide-range of appropriate assessment methods are used to ensure students have achieved the level of knowledge and skill required. Methods include:
The Medicine program is outcome based. The starting point for design was defining the capabilities required of graduates to be able to practise successfully in future medical environments. These eight capabilities include ‘generic’ capabilities such as self-directed learning, teamwork and reflective practice, as well as more traditional medical knowledge and skills. All learning activities and assessments in the program are related to these capabilities and you should use them as a guide when planning your learning.
The capabilities were developed through a process involving literature searches, consultations with other medical schools, and panels of experts. They represent UNSW Medicine’s minimum expectations for the level of achievement of its graduates. The capability indicators are not intended as checklists for performance assessments. Rather, they describe goals and indicate the expected range and depth of acceptable performances. Assessors will be guided by these indicators when judging your work in the program. They will decide whether the work you present for assessment approximates in range and depth to the sorts of performances described in the capability indicators. This allows you considerable freedom to pursue your interests and needs as you develop as a medical professional, within the requirements of each assessment activity, while giving UNSW Medicine a guide to minimum standards.
The eight graduate capabilities to be achieved throughout the program are all equal in importance. They are summarised below to show how each capability develops over the three Phases of the program. There are many elements of knowledge and performance that could easily relate to a number of capabilities. For the sake of convenience in teaching and assessment and to avoid repetition they have generally been assigned to only one capability.
In the tables below, the capabilities have often been abbreviated and/or combined. The Black Dots (·) in the columns indicate an emphasis on the development of the relevant capability. All capabilities are cumulative, so that once developed they are expected to be used and refined in subsequent Phases. The numbers in brackets refer back to the full wording of the capability elements found in a more extensive table of capability elements on the Medicine program website.
http://medprogram.med.unsw.edu.au/graduate-capabilities
|
Applied Knowledge |
Interactional Abilities |
Personal Attributes |
|---|---|---|
|
Using basic and clinical sciences in the practice of medicine |
Effective communication with patients, team members, colleagues and the community |
Self-directed learning and critical evaluation skills |
|
Understanding the social and cultural aspects of health and disease |
Working as a member of a team |
Understanding ethics and legal responsibility in medicine and acting in an ethical and socially responsible manner |
|
Patient assessment and management |
|
Development as a reflective practitioner |
The six-year program is divided into three Phases: scenario based learning, practice based learning and independent reflective learning.
Four domains organise the program throughout the three Phases. Three of these domains represent the stages of the human life cycle, the fourth represents the environment in which life exists.
Within each domain there are four major themes, which are key concepts important to understanding health, illness and medical practice. Themes provide a broad issue for students to explore and students will revisit the theme in different contexts throughout the three Phases.
The content includes aspects of proactive and reactive approaches to health issues in individuals and populations, and is organised into three content streams, biomedical sciences, the social and psychological aspects of health and illness, and medical practice.
Within each Phase, vertical integration occurs with students working together collaboratively. (For example, first and second year students are combined in Phase 1 in the second half of the year.) This means that students play both learner and mentor roles as they progress through Phases 1, 2 and 3.
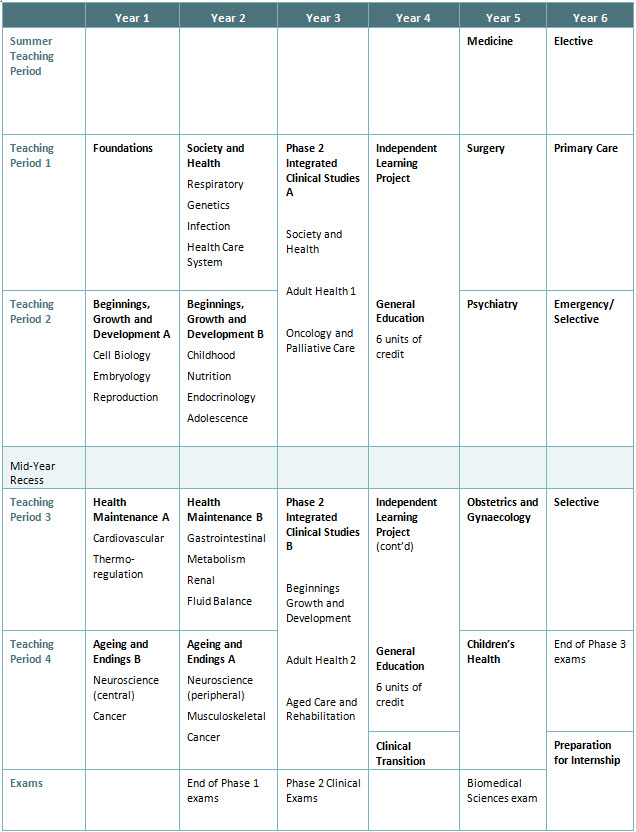
Note: The sequence of courses is illustrative of one possible sequence. Course sequences will vary for individual students.
Within each domain, there are four major themes (see table below). These 16 themes are key over-arching concepts considered critical to understanding health, illness and medical practice.
|
Domain |
Major Themes |
|---|---|
|
Beginnings, Growth and Development |
Conception, pregnancy and birth |
|
Health Maintenance |
Homeostasis, sustenance, and equilibrium |
|
Ageing and Endings |
Menopause |
|
Society and Health |
Society, culture and genes |
The majority of teaching in Phase 1 of the curriculum (first 2 years) occurs on the main university's Kensington campus and includes lectures, small group work, tutorials and practical classes held in laboratories. During this Phase, clinical sessions are held in hospitals.
In Phase 2 of the program (next 2 years), the clinical sessions held in hospitals increase to 3 days per week. Campus teaching (lectures, small group work, tutorials and practical classes) are held on the other 2 days per week at the Kensington campus. Phase 2 also includes the Independent Learning Project. In this unique learning experience, students undertake a supervised research project of their choosing.
In Phase 3 of the program (final 2 years), almost all teaching is conducted in hospitals. It incudes bedside tutorials, classroom tutorials, ward rounds and attendance at clinics. Lectures held on the main university campus also form part of the teaching program in this Phase.
In all three Phases of the program, students will be required to travel to various clinical environments associated with UNSW. These will be the predominant locations for learning in Phases 2 and 3, and will include at least 4 weeks in a non-metropolitan setting and for a quarter of students will include between one and two academic years in a non-metropolitan setting in Phase 2 and/or 3.
The main hospitals located in Sydney used for clinical teaching are:
The main hospitals located outside of Sydney and in rural New South Wales and Victoria used for clinical teaching are:
In addition to the five main rural teaching campuses, the Rural Clinical School utilises the following rural clinical sites:
It is expected that students who gain entry via the Rural Student Entry Scheme will be allocated to a rural hospital and undertake at least either Phase 2 or Phase 3 in rural hospitals. Other local students may have the option or be required to undertake at least either Phase 2 or Phase 3 in rural hospitals and all local students should expect at least 4 weeks in a rural rotation in Phase 3.
Students considering applying for entry into UNSW Medicine must be willing to undertake their training in a range of hospital and health care facilities. For further information please refer to the UNSW Medicine Guidelines on Allocation of Students to Clinical Environments.